Understanding Whether You Need a Neurosurgeon or Orthopedic Surgeon for Spinal Stenosis
A diagnosis of spinal stenosis often brings more questions than answers. One of the most common and important questions patients ask is whether they should be treated by a neurosurgeon or orthopedic surgeon for spinal stenosis. This decision can feel confusing, especially when referrals differ or when patients receive conflicting recommendations.
Spinal stenosis is a complex condition that affects the spinal canal, nerve roots, or spinal cord. Because it involves both neurological structures and the mechanical stability of the spine, care may involve specialists from different medical backgrounds. Understanding how neurosurgeons and orthopedic surgeons approach spinal stenosis helps patients make informed decisions and seek appropriate evaluation, particularly when symptoms progress or treatment plans are unclear. Spinal stenosis is often associated with underlying conditions such as spinal arthritis, spondylosis, spondylolisthesis, and spinal cord compression, which influence both symptoms and treatment decisions.
This guide provides a comprehensive medical overview of spinal stenosis, explains how different specialists manage the condition, and highlights when second opinions play an important role in care.
Understanding Spinal Stenosis and Its Impact on the Body
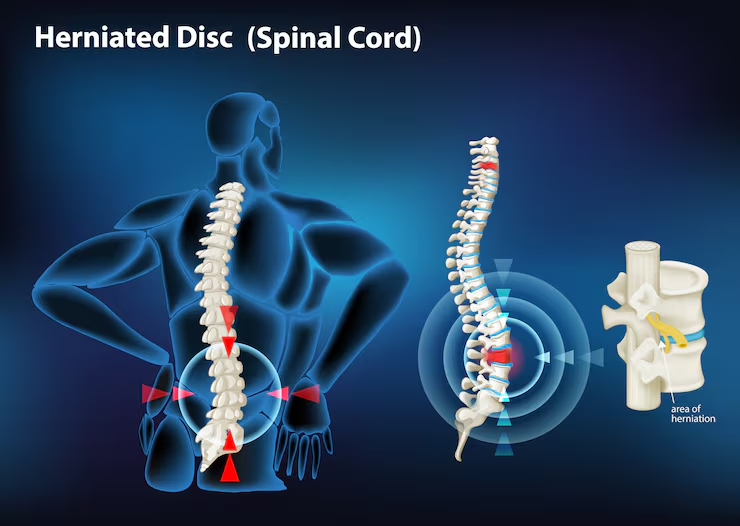
Spinal stenosis refers to narrowing of the spinal canal or the openings where nerves exit the spine. This narrowing reduces space for the spinal cord or nerve roots and can lead to compression. In many cases, stenosis develops slowly as part of the natural aging process, though congenital narrowing, trauma, tumors, or prior spinal surgery may also contribute.Degenerative changes associated with spinal stenosis often include disc degeneration, thickening of spinal ligaments, enlargement of facet joints, and formation of bone spurs. These changes gradually reduce available space for neural structures.
Symptoms depend on the location and severity of stenosis. Cervical spinal stenosis may affect the spinal cord and lead to balance problems, coordination difficulties, or weakness in the arms and hands. Lumbar spinal stenosis commonly causes leg pain, numbness, or difficulty walking. These differences influence whether a neurosurgeon or orthopedic surgeon for spinal stenosis is more appropriate for evaluation and management.
Conditions Commonly Associated With Spinal Stenosis
Spinal stenosis rarely develops in isolation. In most patients, it is the result of progressive degenerative or structural changes within the spine that gradually narrow the spinal canal or nerve passageways. Understanding these related conditions helps clarify why symptoms develop, how spinal stenosis progresses, and why care may involve either a neurosurgeon or orthopedic surgeon for spinal stenosis depending on the underlying pathology.
Spinal Arthritis and Degenerative Joint Changes
Spinal arthritis is one of the most common underlying causes of spinal stenosis. Over time, age-related wear and tear affects the facet joints of the spine, leading to cartilage loss, joint enlargement, and bone spur formation. These changes reduce the available space within the spinal canal and foramina, increasing pressure on nearby nerve structures.
As arthritis progresses, stiffness and inflammation further contribute to narrowing. Patients with spinal arthritis often experience gradual onset of symptoms, which may worsen with activity or prolonged standing. Because arthritis-driven stenosis involves both structural degeneration and potential nerve compression, treatment decisions must consider mechanical stability as well as neurological risk.
Spondylosis and Spondylolisthesis as Structural Contributors
Spondylosis refers to degenerative changes affecting the discs and vertebrae, while spondylolisthesis involves forward slippage of one vertebra over another. Both conditions can significantly contribute to spinal stenosis by altering normal spinal alignment and reducing canal space.
In cases of spondylolisthesis, vertebral slippage may directly compress nerve roots or destabilize the spine, leading to worsening symptoms over time. These structural changes are particularly relevant when evaluating whether orthopedic stabilization or neurosurgical decompression is the primary focus of treatment. The presence of instability often influences surgical planning and specialist involvement.
Spinal Cord Compression and Neurological Impact
Spinal stenosis becomes especially concerning when narrowing leads to spinal cord compression, most commonly in the cervical spine. Compression of the spinal cord can result in symptoms such as balance difficulties, coordination problems, hand weakness, and changes in fine motor control.
Spinal cord compression represents a more advanced and potentially serious manifestation of spinal stenosis. Early recognition is critical, as prolonged compression can result in permanent neurological deficits. In these cases, timely evaluation and intervention are essential to preserve function and prevent further deterioration.
How Spinal Stenosis Is Diagnosed
Diagnosis begins with a detailed clinical history and physical examination. Physicians evaluate pain patterns, neurological function, reflexes, strength, coordination, and gait. Imaging studies such as MRI provide detailed visualization of spinal canal narrowing, nerve compression, disc degeneration, and ligament thickening.
However, imaging alone does not dictate treatment. Many patients show significant narrowing on imaging but have minimal symptoms, while others experience severe symptoms with less dramatic findings. This disconnect is a key reason specialist interpretation matters.
Accurate diagnosis requires correlating imaging findings with clinical symptoms and functional limitations. This process helps determine whether spinal stenosis is clinically significant and whether intervention is necessary.
1. Clinical presentation and symptom progression
The way spinal stenosis presents clinically often guides the decision between a neurosurgeon or orthopedic surgeon for spinal stenosis. Symptoms that indicate neurological involvement require careful attention because they may signal spinal cord or nerve compromise.
- Progressive weakness in the arms or legs
- Numbness or tingling that worsens over time
- Difficulty with balance, coordination, or fine motor skills
When symptoms progress despite conservative care, further evaluation is often necessary. Neurological findings may suggest that neural structures are at risk, which influences specialist selection and urgency of treatment.
2. Structural versus neurological contributors
Spinal stenosis often develops due to a combination of structural degeneration and neural compression. Understanding which factor is dominant helps determine treatment priorities.
- Disc collapse and loss of disc height
- Thickened ligaments narrowing the spinal canal
- Bone spurs encroaching on nerve space
- Spinal instability or alignment changes
When instability or deformity plays a major role, orthopedic spine expertise may be emphasized. When spinal cord or nerve root compression drives symptoms, neurosurgical input is often critical. Many patients fall into an overlap category, reinforcing the importance of comprehensive evaluation.
3. Why imaging findings alone are not enough
MRI and CT scans provide valuable anatomical information, but they do not fully explain symptom severity. Some patients have severe stenosis on imaging but remain relatively functional, while others have disabling symptoms with moderate narrowing.
This mismatch is one reason patients often seek additional evaluation when deciding between a neurosurgeon or orthopedic surgeon for spinal stenosis. Clinical judgment, experience, and careful examination are essential to avoid unnecessary intervention or delayed treatment.
The Neurosurgical Approach to Spinal Stenosis
Neurosurgeons specialize in conditions affecting the nervous system, including the spinal cord and nerve roots. Their training emphasizes protecting neurological structures and addressing conditions that threaten nerve function.
In spinal stenosis, neurosurgeons are commonly involved when spinal cord compression, cervical myelopathy, or progressive neurological deficits are present. Their approach prioritizes precise decompression of neural tissue while minimizing neurological risk.
Cervical spinal stenosis often requires neurosurgical evaluation, particularly when symptoms include hand clumsiness, gait instability, or balance problems. Even subtle spinal cord compression can lead to long-term impairment if left untreated.
Common scenarios evaluated by neurosurgeons
- Cervical stenosis with signs of myelopathy
- Progressive weakness or sensory loss
- Balance or coordination difficulties
- Neurological decline despite conservative treatment
In these situations, surgical timing and technique play a critical role in preserving neurological function and preventing irreversible damage.
The Orthopedic Spine Surgery Perspective
Orthopedic spine surgeons focus on the musculoskeletal system, including spinal alignment, stability, and biomechanics. Their expertise is especially relevant when spinal stenosis is associated with degenerative changes that compromise structural integrity.
Orthopedic surgeons frequently manage spinal stenosis when instability, deformity, or mechanical back pain contributes significantly to symptoms. Their approach emphasizes restoring alignment and maintaining long-term spinal stability.
Modern orthopedic spine surgeons also receive extensive training in neural decompression techniques, allowing them to manage many stenosis cases effectively.
Conditions commonly managed by orthopedic spine specialists
- Degenerative spondylolisthesis
- Spinal deformities such as scoliosis
- Multi-level degenerative disc disease
- Stenosis requiring fusion or stabilization
When maintaining mechanical stability is a primary concern, orthopedic expertise is often central to treatment planning.
Fellowship training and overlap between specialties
In modern spine care, many surgeons complete fellowship training in spine surgery regardless of whether their background is neurosurgery or orthopedics. This advanced training has narrowed traditional differences between specialties.As a result, choosing between a neurosurgeon or orthopedic surgeon for spinal stenosis often depends more on individual experience and case focus than on specialty label alone. Fellowship-trained surgeons frequently perform similar procedures and achieve comparable outcomes.
Not all spinal stenosis requires surgery. Many patients respond well to non-surgical treatments, especially in early or moderate stages.Conservative management may include physical therapy, medications, activity modification, and targeted injections. Both neurosurgeons and orthopedic surgeons assess whether non-surgical care remains appropriate before recommending surgery.Monitoring symptom progression over time helps determine whether surgical thresholds have been reached.
Surgical treatment options for spinal stenosis
When conservative treatment fails or neurological symptoms worsen, surgery may be considered. Surgical goals include relieving pressure on neural structures and maintaining or restoring spinal stability. Procedures may involve decompression alone or decompression combined with fusion. The choice depends on anatomy, symptom severity, and spinal mechanics. Both a neurosurgeon or orthopedic surgeon for spinal stenosis may perform these procedures depending on training and complexity.Research consistently shows that outcomes for spinal stenosis surgery depend more on surgeon experience, case volume, and patient selection than on whether the surgeon is a neurosurgeon or orthopedic surgeon.Specialists who routinely treat spinal stenosis are more likely to recognize subtle findings, select appropriate candidates, and manage complications effectively. This reinforces the importance of expertise over titles.
Second opinions are an important part of spinal stenosis care, particularly when treatment decisions are complex.
- Surgery is recommended but symptoms are mild or intermittent
- Imaging findings do not clearly explain symptoms
- Multiple spinal levels are involved
- Prior spinal surgery complicates anatomy
A second opinion can confirm diagnosis, refine treatment strategy, and provide reassurance.Spinal stenosis often progresses slowly, allowing time for thoughtful evaluation. Second opinions provide an additional perspective, especially when neurological and structural factors overlap.They help ensure that treatment recommendations align with both current symptoms and long-term outcomes.
Long-Term Outcomes of Spinal Stenosis Treatment
Understanding long-term outcomes is essential when deciding between a neurosurgeon or orthopedic surgeon for spinal stenosis. While short-term symptom relief is often the initial focus, long-term spinal health, neurological preservation, and functional independence are equally important considerations.Patients treated conservatively may experience stable symptoms for years, particularly when stenosis is mild and neurological function remains intact. However, progressive narrowing of the spinal canal can eventually lead to worsening nerve compression. This is why long-term monitoring plays a crucial role, even when surgery is not immediately recommended.
For patients who undergo surgery, outcomes depend on several variables, including the severity and duration of symptoms before intervention, the presence of neurological deficits, and overall spinal stability. Early surgical intervention in appropriately selected patients often leads to better neurological recovery, while delayed treatment may limit the extent of symptom improvement.
How Delayed Treatment Can Affect Neurological Recovery
One of the most important reasons physicians carefully evaluate whether a patient should see a neurosurgeon or orthopedic surgeon for spinal stenosis is the risk of permanent neurological damage. Prolonged compression of neural structures can lead to irreversible changes, even if decompression is later performed.In cervical spinal stenosis, delayed treatment can result in persistent balance problems, coordination difficulties, and weakness that may not fully resolve after surgery. Lumbar stenosis, while less likely to cause spinal cord injury, can still lead to chronic nerve damage that affects walking tolerance and lower-extremity strength.
This is why timely evaluation, close monitoring, and appropriate specialist involvement are critical. Patients who notice worsening symptoms over time should not assume that progression is inevitable or untreatable.
Individualized Decision-Making in Complex Spine Cases
Spinal stenosis rarely presents as a simple, isolated condition. Many patients have coexisting spinal issues such as disc degeneration, arthritis, scoliosis, or prior surgical changes. These complexities influence whether management is best handled by a neurosurgeon or orthopedic surgeon for spinal stenosis.
Individualized decision-making considers:
- Overall spinal alignment and biomechanics
- Neurological examination findings
- Functional limitations in daily life
- Patient age, activity level, and health status
A personalized approach ensures that treatment recommendations align with both current symptoms and long-term quality of life goals. This is particularly important for patients with multi-level stenosis or prior spine surgery.
The Role of Multidisciplinary Spine Care
In modern spine care, collaboration between specialists is increasingly common. Many complex spinal stenosis cases benefit from input from both neurosurgical and orthopedic perspectives. This multidisciplinary approach allows for comprehensive evaluation of neurological and structural factors.When neurosurgeons and orthopedic spine surgeons collaborate, treatment plans often become more refined and balanced. This collaboration reduces the risk of overtreatment while ensuring that neurological safety is prioritized when needed.Patients who seek care at centers that emphasize collaborative spine evaluation may benefit from broader expertise and more nuanced treatment planning.
Why Second Opinions Are Especially Important in Spinal Stenosis
Second opinions play a vital role in spinal stenosis management, especially when surgical decisions are involved. Choosing between a neurosurgeon or orthopedic surgeon for spinal stenosis can feel overwhelming, particularly when recommendations differ or when surgery is presented as the only option.
A second opinion can help patients:
- Confirm whether surgery is truly necessary
- Understand alternative treatment pathways
- Clarify the risks and benefits of different surgical approaches
- Gain confidence in their treatment plan
In many cases, second opinions either reinforce the original recommendation or offer a less invasive alternative that was not previously discussed.Not all spinal stenosis cases progress at the same rate. Some patients experience stable symptoms for long periods, while others worsen more rapidly. Borderline cases, where symptoms are present but not clearly severe, are ideal candidates for second opinions.
In these situations, additional evaluation can help determine whether close observation, conservative treatment, or early intervention is most appropriate. This measured approach reduces unnecessary procedures while ensuring that worsening neurological signs are not overlooked.
Psychological and Quality-of-Life Considerations
Spinal stenosis affects more than just physical function. Chronic pain, limited mobility, and uncertainty about treatment decisions can significantly impact mental well-being. Anxiety and fear often arise when patients are unsure whether they are making the right choice between a neurosurgeon or orthopedic surgeon for spinal stenosis.
Clear explanations, realistic expectations, and shared decision-making help reduce emotional stress. Patients who feel informed and involved in their care tend to report higher satisfaction, regardless of whether treatment is surgical or non-surgical.
Recovery Expectations After Treatment
Recovery timelines vary depending on treatment approach, severity of stenosis, and individual health factors. Patients managed conservatively may focus on gradual symptom control and functional adaptation. Those undergoing surgery may experience phased recovery, with early pain relief followed by gradual improvement in strength and mobility.
Understanding recovery expectations before treatment helps patients prepare physically and mentally. This is another area where detailed discussions and second opinions can provide clarity and reassurance. Long-term follow-up is an essential component of spinal stenosis care. Even after successful treatment, ongoing monitoring helps detect changes early and address new symptoms promptly.
Follow-up evaluations often include periodic imaging, neurological assessments, and functional evaluations. This proactive approach supports long-term spinal health and helps maintain quality of life.
Final Thoughts on Choosing the Right Specialist
Deciding between a neurosurgeon or orthopedic surgeon for spinal stenosis is not about choosing one specialty over another. It is about selecting the right expertise for the specific characteristics of the condition.
Patients benefit most when decisions are guided by:
- Symptom severity and progression
- Neurological involvement
- Structural stability of the spine
- Surgeon experience and focus
In many cases, seeking a second opinion provides the clarity needed to move forward confidently. An informed, individualized approach ensures that treatment decisions prioritize both immediate relief and long-term outcomes.