- (213) 369-4583
- Monday - Friday
- 9 am - 5 pm
Normal Pressure Hydrocephalus: Diagnosis and Treatment

Apr 13, 2022
Do you feel difficulty in walking and maintaining balance? Are you worried about your ongoing memory loss and progressive loss of thinking and reasoning skills? Is there always a frequent urge to micturate? You think it is Normal Pressure Hydrocephalus (NPH) but it might not be.
It is difficult to know how many people have NPH syndrome because its symptoms are very much similar to Alzheimer’s and Parkinson’s disease. However, an experienced doctor familiar with these conditions can differentiate between them and tell if you have NPH or not.
You can read this blog to be in a better position to tell if you have Normal Pressure Hydrocephalus. Moreover, we will also enlist a couple of procedures used to treat NPH that you can adopt after discussing with your doctor.
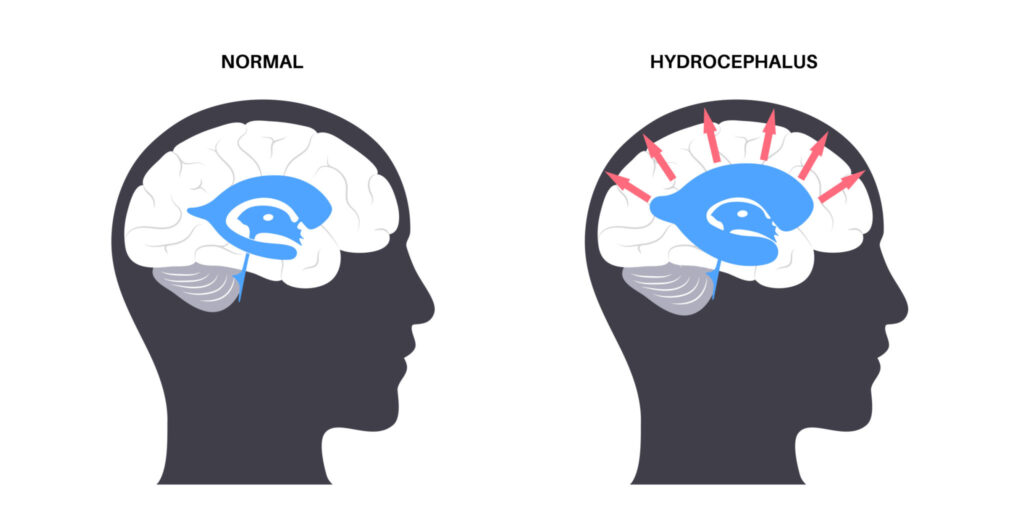
What is normal pressure hydrocephalus syndrome?
Your brain has multiple chambers called ventricles that contain cerebrospinal fluid (CSF) that cushions your brain and spinal cord. Normally the production and absorption of CSF are well balanced within the body, but sometimes due to idiopathic causes excessive fluid accumulates in the ventricles as a result they enlarge and exert pressure on nearby brain tissues. This condition is known as Normal Pressure Hydrocephalus syndrome. It decreases the efficiency of the brain which leads to thinking and reasoning problems, difficulty walking, and loss of bladder control. NPH is more common in adults of age 60 years or older compared with young people.
You may also want to read: Who Is a Neurosurgeon and When Do You Need One?
Who is at risk?
- A person of 60 years of age or older.
- Have had any head injuries.
- A person with existing neurological problems like infections or tumors.
Symptoms of normal pressure hydrocephalus syndrome
It exhibits a classic triad of clinical findings that consists of
- Gait deviation
- Dementia( memory loss)
- Urinary incontinence
Other includes
- Difficulty walking feels as if feet are stuck or glued to the ground
- Reduced concentration
- Impaired planning and decision making
- Frequent falls on the ground due to poor balance
- Difficulty responding to questions.
- Depression
Diagnosis of Normal Pressure Hydrocephalus
Mostly it’s an on-spot clinical diagnosis. But since it’s a rare disorder overlapping with many other similar conditions, the definitive diagnosis could only be made through radiological findings.
Following are the tests often used by the doctors for the diagnosis of Normal Pressure Hydrocephalus.
Imaging tests
Under these tests, brain CT Scan or MRI is are conducted to look for enlarged ventricles.
Lumbar puncture
Under local anesthesia, a thin needle is passed in the lower back in the spinal fluid space to take out some CSF. The fluid is then analyzed to see if symptoms are temporarily relieved and the CSF pressure is also measured.
Gait analysis
It’s a timed walk test. The patient is observed as he walks about 30 feet to look for any gait or balance abnormality.
Neurophysiological testing
A Series of assessments are conducted to know if there is a loss of brain functions including memory, concentration, and cognition.
What is the treatment of Normal Pressure Hydrocephalus?
If NPH is diagnosed in the early stages, there is a chance of complete recovery. Since, there is little use of medications in Hydrocephalus, the most appropriate treatment is surgery that involves placing a tube (known as Shunt) in the patient's body to drain the excess fluid. The prognosis of any surgery relies on the patient's general health and stage of the disease.
There are two methods used either to divert the excess CSF away from the brain or to directly remove the cause of obstruction.
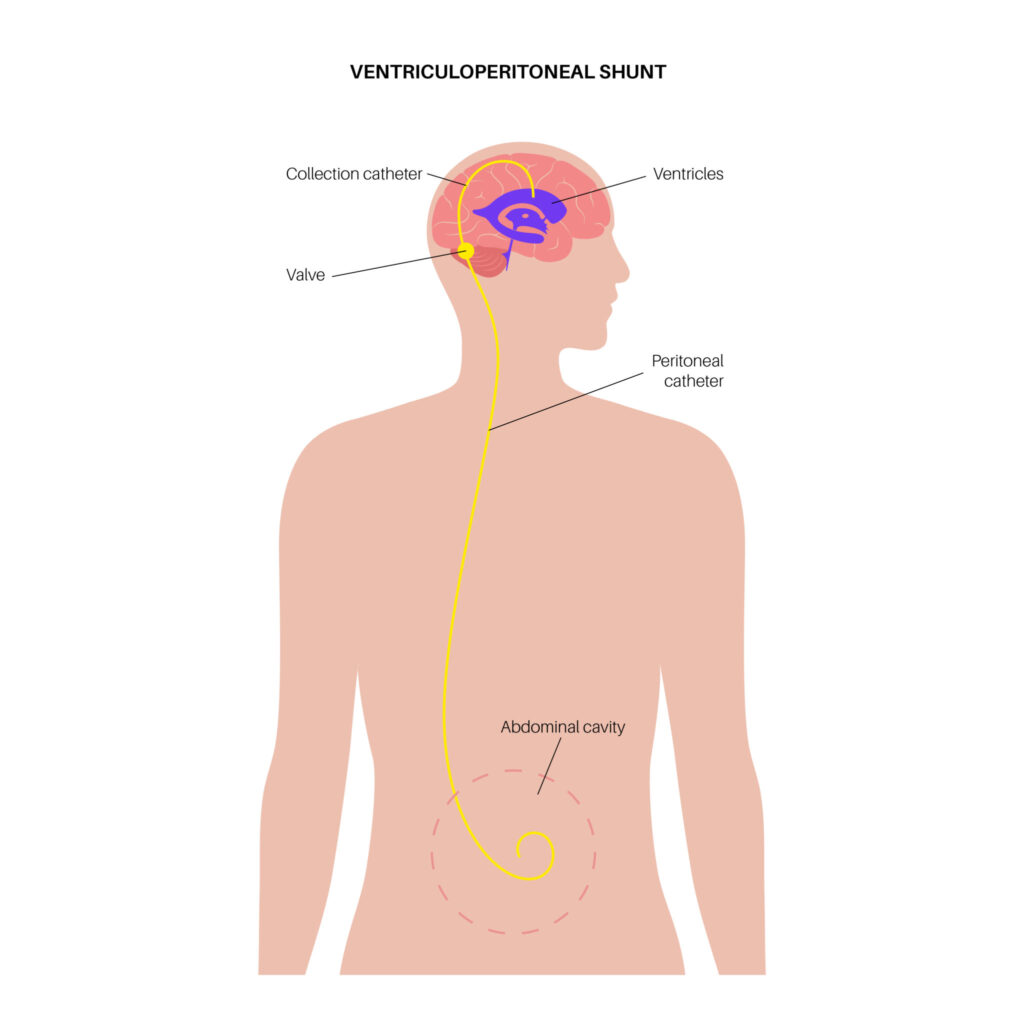
Shunt system
The tube placed in the brain is called a ventriculoperitoneal shunt, it’s a flexible tube along with a catheter and valve placed under the patient’s skin to drain excess CSF from a ventricle inside the brain. It is then passed from the head through the neck and chest to another cavity such as the peritoneal cavity (the area surrounding the abdominal organs) or a heart chamber where the excess fluid can be more easily absorbed by the body.
People with Hydrocephalus usually need this shunt system throughout the rest of their lives and require regular monitoring as well.
Endoscopic Third Ventriculostomy
This procedure works for a limited number of people. The surgeon makes a hole in the bottom of one of the ventricles or between the ventricles with the help of a tiny camera using fiber optics. It allows CSF to flow out of the brain and the doctor can see the activity on the screen. This procedure usually provides good results mainly for those with short-duration symptoms.
Recovery and follow up visits
Recovery from any surgery depends upon the patient's general health and how far the disease has progressed. Once inserted, Shunt usually remains inside the body throughout the patient's life. The shunt continuously performs its function of diverting CSF away from the brain.
Neurological functions are evaluated after surgery, if any neurological problems persist then rehabilitation is required for further improvement.
Long-term follow-ups by a doctor are required and diagnostic tests are done from time to time to see if the shunt is working properly or not.
Get in touch with a Neurosurgeon
You don’t need to worry about your symptoms. Get in touch with a neurosurgeon as early as you can if you or any of your elderly relatives are experiencing these symptoms. The earlier the Hydrocephalus is diagnosed, the better the chance of successful treatment. Considering making an appointment? Contact the spine experts at Southern California Brain and Spine Surgery today. Our board-certified neurosurgeon, Dr. Moksha Ranasinghe will make an appropriate management plan for you!
For more information, you can schedule an appointment by clicking the contact button or call us at (213) 369-4583 to speak to someone at the clinic.